Importantly, having medicare coverage is key to having health fund coverage, which reduced the overall cost from $25,000 out of pocket to $15,000 when you choose dr moncrieff for your tummy tuck. Benefits application this medical policy relates only to the services or supplies described herein.
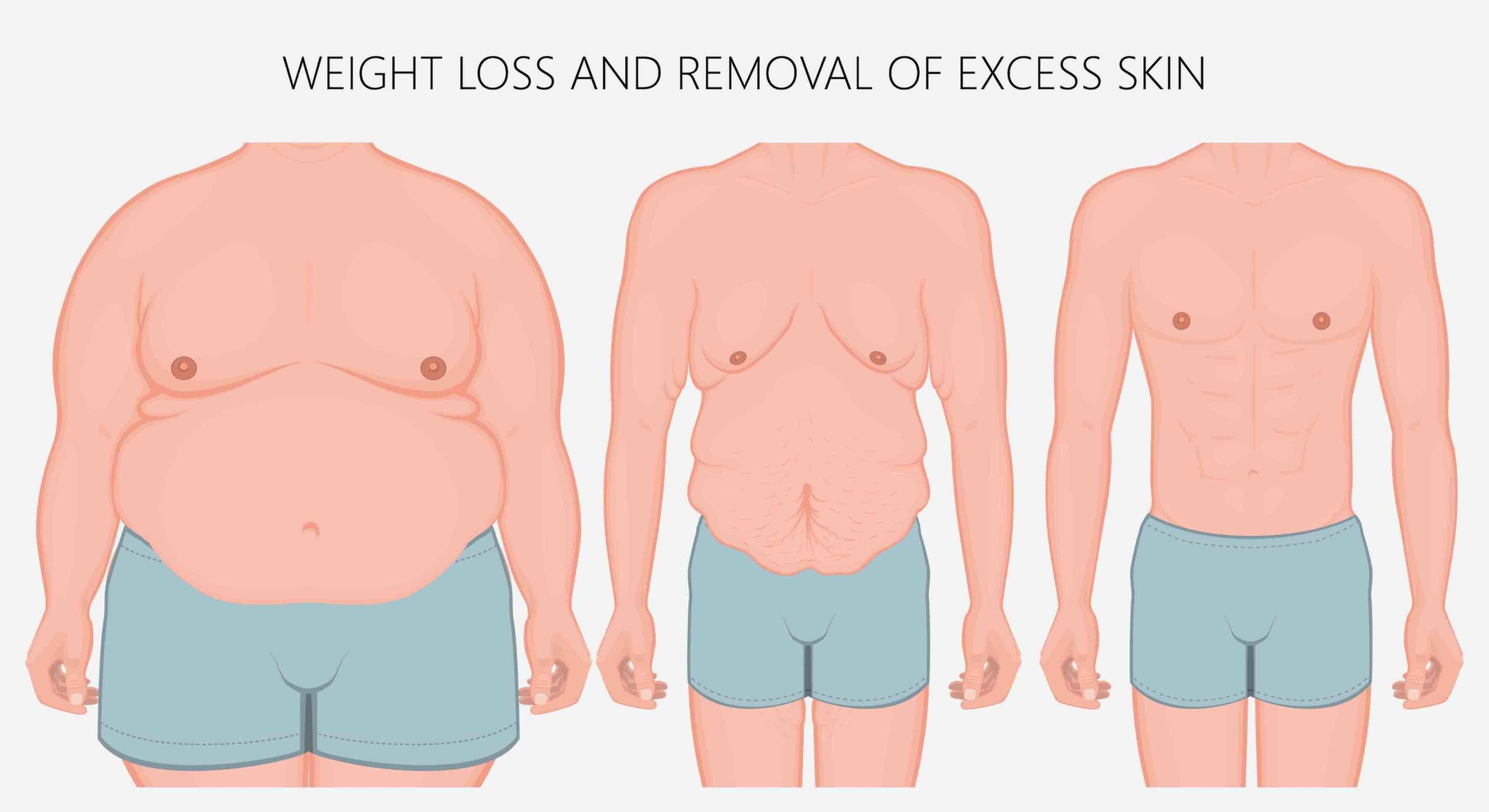
Does Health Insurance Cover Excess Skin Removal All
However, medicare will provide a modest rebate if you satisfy the weight loss criteria introduced in 2016.

How to get a panniculectomy covered by medicare. If your procedure requires prior authorization before medicare will pay for it, you don’t need to do anything. In addition, panniculectomy billed at the same time as an open abdominal surgery, or if is incidental to another procedure, is not separately coded per coding guidelines. When a panniculectomy is being performed at the same time as bariatric surgery.
If your procedure requires prior authorization before medicare will pay for it, you don’t need to do anything. How to get a panniculectomy covered by medicare. There are no published medicare guidelines for “medical necessity” regarding abdominoplasty/panniculectomy.
The panniculus, when present, is the primary cause of skin conditions such as cellulitis requiring systemic antibiotics or Indications for coverage the following are eligible for coverage when the below criteria are met. Medicare covers panniculectomy when it’s a medical need.
Because abdominal panniculectomy surgery is often covered by medicare even with a small surgical deductible, it is often used to save money. Panniculectomy when all of the following criteria have been met: In some cases, you pay first and get a reimbursement.
A surgeon must do the procedure and then wait and see if medicare will actually approve (pay) for the procedure. This is the removal of the pannus. This forwardhealth update introduces new pa approval criteria for panniculectomy and lipectomy surgeries effective for pa requests received on and after february 3, 2014.
Will united healthcare cover a panniculectomy? Any serious need for the removal of skin has coverage. When it comes to an abdominal panniculectomy, no matter how medically indicated it might be (and your mother certainly fulfills.
Coverage for investigational or not medically necessary services or procedures. To get a panniculectomy approved by insurance most insurance companies require that certain things be documented to prove medical necessity rather than a purely cosmetic reason for performing the procedure. Panniculus hangs at or below symphysis pubis;
When a panniculectomy is being performed to prevent hernia occurrence or to prevent hernia recurrence in conjunction with a hernia repair, unless the member meets the criteria for panniculectomy stated in section ii. Panniculectomy billed for cosmetic purposes will not be deemed medically necessary. Bcbsnc will provide coverage for panniculectomy when it is determined to be medically necessary because the medical criteria and guidelines shown below are met.
There is no rule to define cost or coverage prior to plastic surgery. If excess skin makes your daily life tough, talk to your doctor. However, those used by blue cross of kansas are helpful to review, as these are fairly standard insurance coverage guidelines.
Even if these coverage guidelines are met, medicare may still deny coverage. Panniculectomy and lipectomy surgeries are covered by forwardhealth with prior authorization (pa). These criteria often include documentation of a rash in the skin folds.
Medicare, a federal program, does not preauthorize or preapprove any surgical procedure.